Pleasure, pain activate same part of brain
New finding may lead to better painkillers
Scientists have found pain in the same brain circuits that give you pleasure. That won’t make you cry until you laugh, but it’s likely to lead to better ways to measure and treat chronic pain.
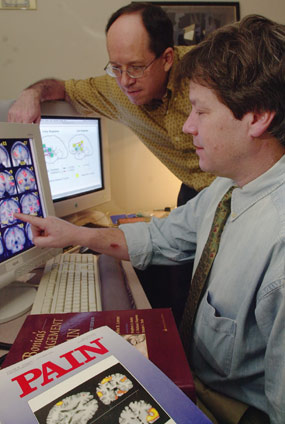
Frustrated by not being able to help patients with unremitting pain, David Borsook, associate professor of radiology at Harvard Medical School, decided to see precisely what happens in people’s brains when they feel pain. Working with Assistant Professor of Radiology Lino Becerra, Hans Brieter, and other colleagues at Massachusetts General Hospital, he heated the hands of eight volunteers enough to hurt, while they underwent brain scanning. The scans showed activity not only in brain regions typically associated with pain but also in those devoted to enjoying pleasurable things like food, drugs, and sex.
This new pain register provides, for the first time, a way to objectively assess chronic pain, the researchers say. Instead of asking a patient to rate her or his pain on a subjective scale of 1-to-10, physicians can obtain a direct measurement from the brain. “By defining brain circuitry that’s specific to the type of distress a patients feels, we can determine the best treatment,” Borsook notes.
Instead of dealing with general complaints of stomach or chest distress, doctors may be able to determine if the hurt comes from the pancreas, the heart, or some other organ. When people come to an emergency room with what they think is a heart attack, doctors need to ascertain whether an ache or twinge actually originates in the heart or, for example, in the esophagus.
In the future, such pain evaluations may influence workmen’s compensation decisions about disability benefits, and detect if a patient is faking pain to obtain drugs.
“I’m absolutely confident,” says Borsook, “that in three to five years, ordering a (brain) image for pain patients will be as routine as a blood test.”
Getting better treatment
One of the first applications of this discovery could be as a tool to evaluate pain medications. Morphine and other opiates, for example, have effects on the body that go beyond alleviating pain. Do these help the hurt, or do they produce unnecessary side effects?
“Functional brain scans can tell which drugs are the best painkillers,” Borsook says. As opposed to producing images of bones, tumors, and other structures, functional magnetic resonance scanning detects what is happening in terms of how the brain functions.
While undergoing such scans, eight volunteers had their hands gently warmed or painfully heated. First, they were exposed for 25 seconds to a temperature of 106 degrees F, just below the level at which pain fibers in all mammals, from mice to humans, become activated. During subsequent scans, heat was increased to 115 degrees F, which produces a burning feeling without causing skin damage.
The resulting sensations of heat were expected to activate only well-known circuits deep in the center of the brain, some of which release natural painkillers. It did. But in the seconds before these circuits switched on, the experimenters saw activity in the area that usually responds to rewards such as money, good food, and sex.
That area, called the nucleus accumbens, sits closer to the front of the brain than the previously mapped pain sensors. Experiments done by others at Massachusetts General Hospital and elsewhere show that this small region lights up when people and animals experience pleasurable sensations ranging from tasty food to the sight of a beautiful face.
In more recent experiments, results of which have not yet been published, Borsook and his colleagues gave low doses of morphine to healthy volunteers and found that this also stimulated activity in the nucleus accumbens. Together with other work done by Hans Brieter and his colleagues at Massachusetts General Hospital, these studies demonstrate, for the first time, the existence of a single, subconscious system that responds to a continuum of emotions from pain to pleasure.
“At present, all pain treatments are based on the classic sensory circuits that respond by activating the release of natural analgesics (painkillers),” Borsook comments. “Discovery of emotional circuits could well be the key to defining new targets for treating chronic pain.”
Pain becomes a disease
Borsook and his team only tested men. Pain activates the same circuits in both sexes, but levels of such activity rise and fall during the menstrual cycle. The investigators plan more tests and analyses to pin down these female variations.
An estimated 40 million men and women in the United States suffer chronic pain, defined as continuous aching lasting longer than six months. Such people run a high risk of becoming anxious, depressed, and even suicidal. They go from specialist to specialist to find relief, often without success. Unable to provide help, the doctors become frustrated. “Treating chronic pain patients is something few physicians want to do,” Borsook comments.
“Pain can transform a normal brain into an abnormal one,” he continues. “Pain becomes not just the symptom of disease but a disease itself.”
Understanding the relationship between emotional and sensory circuits in the brain offers hope of finding new ways to treat this kind of pain. Borsook thinks of it as “an alteration of the pain-pleasure continuum. Things that previously were pleasant and rewarding may no longer be so when a person is in chronic pain. We need to find ways to rebalance that circuitry.”
Such imbalances can also go in the other direction. Borsook recalls so-called psychosurgery treatments in the late 1950s to early 1960s wherein small parts of the brain were destroyed to relieve chronic pain. He met eight of these patients, and they all said the same thing: “The pain is the same but now I don’t care.”
“It was a very profound statement,” Borsook believes, “because it reveals a disconnect between the emotional and cognitive parts of pain circuitry. It shows that there is both a feeling and a thinking system that receives information about pain. Our recent experiments demonstrate that the feeling part is activated first. We feel pain before we think about it.”
Borsook himself is haunted by the phantom of pain. Many years ago, he lost the tip of a finger, and he still feels “a painful, tingling sensation,” particularly when the finger is exposed to cold temperatures. That experience makes him sympathetic to people with chronic pain, and he has spent most of his medical career trying to help them.
In a lecture to Harvard Medical School students, Borsook brought with him a patient who had developed chronic pain in his arm as a result of surgery for carpal tunnel syndrome. He had been seeing Borsook for five to six years, but the doctor was not able to help him.
“Why do you still see Dr. Borsook?” One student asked.
“My visits provide me with the hope that help will come eventually,” he answered. “The regular interaction with a doctor who tries to help me provides some kind of control in my life, some order in my treatment.”
“If it was simply a matter of health-care accounting, the patient would get rid of me,” Borsook comments. “But it’s more than that. I was providing a place of refuge and hope.”
With their new discovery about the pain’s effect on the brain, Borsook and his colleagues expect to be able to do more for such patients in the near future.
Sweet is pleasure after pain. – Dryden